Category Archives: visceral
chirugia addominale e toracica
laparoendoscopic rendezvous in the management of cholecystocholedocholithiasis








laparoscopic appendectomy vs open procedure.EBM
Quest’opera è distribuita con Licenza Creative Commons Attribuzione – Non commerciale – Non opere derivate 4.0 Internazionale.
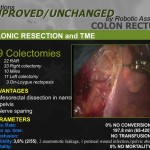
colon mininvasivo

Quest’opera è distribuita con Licenza Creative Commons Attribuzione – Non commerciale – Non opere derivate 3.0 Italia.
“rendez vous” endolaparoscopico nella colecisto-coledoco litiasi
ENDOLAPAROSCOPIC “RENDEZ VOUS” PROCEDURE.OUR EXPERIENCE IN THE TREATMENT OF CHOLECYSTO-CHOLEDOCHOLITHIASIS.
Luca Felicioni MD General and Minimallyinvasive Surgery “Misericordia”Hospital Grosseto ITA
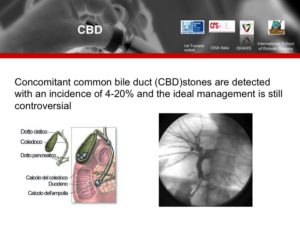
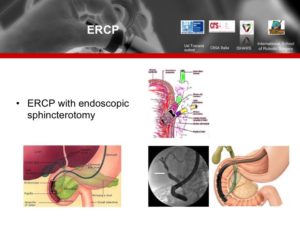
The advent of endoscopic and laparoscopic techniques changed surgery in many ways.For the management of cholelithiasis, laparoscopic cholecystectomy(LC)is the treatment of choise.There is still some controversy regarding the optimal timing and best method for the removal of common bile duct stones(CBDS).A number of different methods for the management of common bile duct stones (CBDS) have been proposed and are currently in clinical use including endoscopic sphinterotomy (ES) before LC in patients with suspected common bile duct stones,laparoscopic bile duct exploration and postoperative endoscopic retrograde cholangiopancreatography (ERCP).Also the alternative technique of peroperative ES is emerging.
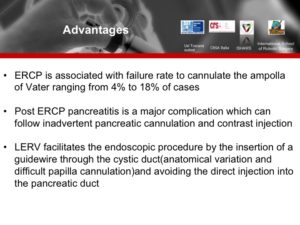
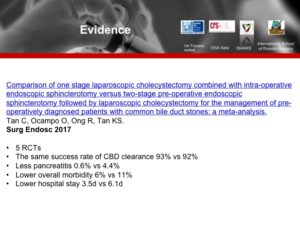
Since the introduction of laparoscopic cholecystectomy (LC),the frequency of pre- as well as postoperative removal of CBDS by ERCP has increased.A major concern regarding both pre- and postoperative extraction of CBDS by the ERCP techniques is the risk for development of pancreatitis,which in recent prospective studies varied between1% and 13.5% after an ERCP procedure.Therefore efforts should be made to minimize the number of unnecessary preoperative ERCP.Only 27%-54% of patients suspected by clinical,biochemical and radiological criteria effectively show common bile duct calculi,therefore a high number of patients undergoing unnecessary ERCP are exposed to a considerable rate of complications.Postoperative ERCP and ES,with the clear advantage of limiting ERCP to documented cases of CBD calculi but with a failure rate of approximately 2%-15%,in which case a further procedure to clear CBD is necessary.Laparoscopic stone removal by either the trancystic approach (small stones) or by common bile duct exploration (CBDE) via a choledochotomy,allows for a more selective approach to the removal of CBDS,and thus the avoidance of unnecessary preoperative ERCP.Laparoscopic transcystic CBD exploration (LTCCBDE)by Dormia basket and/or 8mm Fogarthy angioplasty catheter is effective in approximately 70-90% of cases.Laparoscopic CBD exploration through choledochotomy (LCBDE) is effective in 50-97% of cases and in any case tehnically demanding and time-consuming.The intraoperative approach, in spite of all that, benefits the patient by reducing treatment from a two-step procedure to single-step procedure under general anesthesia.Intraoperative ERCP moreover can be more readily incorporated into daily clinical practice because of its easier learning curve.
In an attempt to minimize the risk for induction of pancreatitis and avoid unnecessary exploration of the CBD,we have adopted a method for removing CBDS intraoperatively by ERCP.We report our experience during the last 5 years of combining LC with IO-ERCP,using a modified version of the techniques previously described in the literature.
Materials and methods
All patients admitted with symptomatic cholelithiasis were studied with ultrasound (US) and liver function tests.CBD stones were suspected when three or more of the following findings were present:dilatation of CBD>7mm or elevation of the liver function tests for bilirubin ,GGT,ALP,AST,ALT and amylase.In this case the endoscopic team was alerted to possible need for peroperative ERC.TC scan or Magnetic Resonance Cholangio pancreatography (MRCPA) have been used to detect or confirm CBDS preoperatively.
Patients underwent LC without routine intraoperative cholangiography (IOC).In our group of 81 patients scheduled for rendez vous procedure 75 IOC were performed. When IOC demonstrated or confirmed the presence of CBDS,a peroperative ERCP and ES were attempted.A duodenoscope and essential accessory equipment were brought to the operating room by the endoscopist.While waiting for the endoscopist to arrive, the surgeon introduced a 0.025-or 0.035-in guide-wire into the cystic duct (Jagwire High Performance Guidewire Boston Scientific)and advanced the guidewire down through the sphincter of Oddi and into the duodenum,if possible,usually through the IOC catheter (Chevassou 6Fr) inserted through a right ipocondrio transwall iv cannula.The IOC catheter is assured at the cystic duct by a 10mm endoclip.At the beginning of the endoscopic procedure the guidewire was caght by a polypectomy snare and pulled through the working channel of the duodenoscope.This maneuver requires cooperation between the surgeon and the endoscopist so that the guidewire is advanced without causing tension on the duodenal wall.A sphincterotome was introduced over the guidewire and into the bile duct.The guidewire greatly facilitated cannulation of the bile duct.Contrast (Omnipaque;Nycomed,Norway) was administered through the sphincterotome to perform endoscopic retrograde cholangiography (ERC).When a CBDS was identified a sphincterotomy was carried out.A retrieval balloon or a stone retrieval basket was then used to remove the stone(s).If the CBD could not be cleared of stones or in laborious periampullary manoeuvres an endoscopic naso-biliary stent was introduced to secure the bile flow.At the end of each ERC,care was taken to remove all of the gas from the stomach so as to facilitate the completion of the LC.
Between January 2003 and October 2008 ,81 patients (34 male and 47 famale) underwent laparoscopic cholecystectomy with planned peroperative ERCP at “Misericordia” Hospital,General and Minimally invasive Surgery department for symptomatic cholelithiasis and suspected or demonstrated choledocolithiasis.The median age was 61.1years(range23-86,SD17.5).In this series, 73 patients with CBDS or ampullar sclerosis demonstrated by IOC underwent peroperative ERCP and ES with the described technique,whereas 8 patients were treated by ERCP+ES without the transampullar guidewire.ES and CBD clearance was successful in 75 of 79 cases with single-staged surgery and in all cases treated in two steps or converted.2 paients planned for the single-staged procedure required conversion to open surgery during cholecystectomy for iatrogenic lesion of CBD or iperinsuflation.In 8 patients the guidewire could not be passed through the cystic duct into the duodenum,but retrograde CBD cannulation was possible without guidewire in 7 cases with cannulation frequency of 98.7%.The mean operating time was 152.5min(range, 60-360;SD +-46.8) decreased from the mean time of 221.2min during the 1st year of the study ,to the mean time of 139.5min during the 5th year.The mean bleeding rate was(ml)40.8+-10.2.The mean postoperative Hospital stay was 7.1days (range2-24;SD +-2.1) with a series of patients admited in internistic ward and with a second series admited in surgical ward .No patient was readmitted after the procedure within 30 days.The combined procedure of cholecystectomy with IO-ERCP yielded a complete removal of stones in 75 of 79 patients( 94.9%).Endoscopic sphincterotomy (EST) followed by naso biliary tube was performed in 14 patients in the early fase of the learning curve of the endoscopic staff or when the CBD clearance was no completely convincing. 2 patients were treated in two steps with postoperative ERCP.The ERCP related complications were: one mild bleeding from the papilla (managed without endoscopic adrenaline injection),3 raised serumamylase resolved spontaneously with no symptoms,6 raised serumbilirubin resolved spontaneously.No patients developed postoperative pancreatitis,cholangitis or perforation related to the Rendez Vous procedure.Only one patient with retrograde CBD cannulation without guidewire died after a postoperative severe acute pancreatitis.Prophylactic antibiotics, and peroperatory gabesato mesilato 100mgx10 and somatostatina 3mgx2 were given to all patients scheduled to undergo IO-ERCP.
Discussion
Although laparoscopic cholecystectomy has become the treatment of choice for symptomatic cholelithiasis, the optimal minimally invasive management of CBDS remains controversial, with many different treatment options employed throughout the world. Peroperative management of CBDS involves the use of ERCP for diagnosis and the creation of a sphincterotomy, with stone extraction if stones are found. Patients with symptomatic cholelithiasis are usually selected for this procedure based on laboratory values (e.g., elevation of the liver function tests) and/or ultrasound results (e.g., a dilated CBD). ERCP is performed either as an outpatient procedure or during admission for LC.
Preoperative ERCP can be effectively used to confirm the presence of stones and treat patients with unequivocal signs of CBDS; however, even with the best selection criteria, only up to one-third of patients undergoing preoperative ERCP will demonstrate choledocholithiasis. This represents an unnecessary risk to patients who do not have choledocholithiasis and a substantial cost. Furthermore, preoperative ERCP, either as an outpatient procedure or during admission for LC stilI requires two separate procedures, which adds additional cost and risk to the patien.Alternatively, patients who are found to have common duct, stones on an intraoperative cholangiogam can be treated by a postoperative ES and stone extraction. This option is much more attractive than open exploration, but it also has drawbacks. The patient is required to have an additional procedure with its associated morbidity and mortality’. Furthermore, the failure rate for postoperative ERCP ranges from 7 to 14%. These failures necessitate another procedure for stone extraction and represent more unnecessary risk and cost to the patient.
Peroperative ES during LC provides an important approach to the management of choledocholitiasis. The single-staged procedure (LC + ERCP) has several advantages:
I. Selecting patients far IOC eliminates unnecessary preoperative ERCP.
2. It reduces patient discomfort and total cost avoiding separate procedures and separate hospital admission.
3. It allows immediate conversion under the same anesthesia to open surgery in case of ERCP failure.
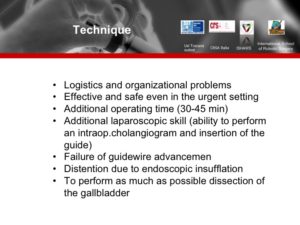
4.The introduction of a guidewire through the cystic duct into the duodenum facilitates ERCP and allows a safer ES.Intraoperative ERCP is not without problems . Disadvantages of peroperative ES are prolongation of the operation time and the logistic problems of organizing the procedure. Much of this extra time is spent setting up the equipment required far ERCP.
The major complication of peroperative ES is acute pancreatitis,although it is generally of mild grade.
This is related to inadvertent cannulation of the pancreatic duct, and only rarely associated with cannulation of the papilla. The use of a guidewire, allowing an anterograde cannulation of the papilla, avoids the risk of inadvertent cannulation of the pancreatic duct, with possible related complications.Our case of severe acute pancreatitis was connected with a failure in the transampullary guidewire crossing and performing a retrograde ERCP.The patient developed a septic pancreatic necrosis in 5th postop day with laparotomy,necrosectomy and jejunostomy.He died in 56th postoperative day for sepsis. We consider that case a complication of ERCP procedure without rendez vous.One patient was discharged in 24th postoperative day after a successfull rendez vous procedure,iatrogenic lesion of CBD and hepatic-jejunostomy.We consider that case a complication of LC but the postop hospital stay is included in our group.
Laparoscopic transcystic duct exploration or laparoscopic choledochotomy and duct exploration are alternative methods of duct clearance. Transcystic duct exploration should always be attempted first, but it may result unsuccessful in narrow cystic ducts.
Laparoscopic choledochotomy and duct exploration have the disadvantage of requiring a T-tube drainage to avoid the risk of CBD stenosis. Primary CBD closure without drainage may be feasible in expert hands, accepting the possible risk of stenosis; however, the handling of a T-tube laparoscopically is more time demanding.A recent meta-analysis by Clayton ESJ confirm that ERCP or laparoscopic surgical CD exploration are equivalent treatments in terms of duct clearance,mortality and overall morbidity although the laparoscopic technique may be more cost effective.A recent survey of general surgeons practising in the USA showed that only 22% actually did so routinely.We have only sporadic experiences.
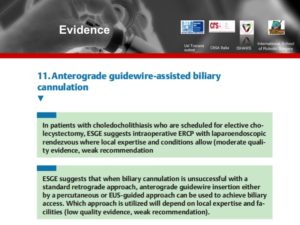
For all these reasons,peroperative ERCP+ ES with rendez vous technique should be the first choise for clearance of the CBD.In case it is not possible to organize the proceduresto be performed at the same time, a postoperative attempt of ERCP over a guidewire inserted into a transcystic drain should be the second choice.
The use of a guidewire for retrograde CBD cannulation in our series allowed CBDS clearance in all cases, whereas the conventional technique of cannulation may produce a high rate of cannulation failure (14% to 23%).
15 patients were scheduled for rendez vous procedure after pancreatitis(mild to moderate acute pancreatitis) and we have compared our global data with this subgroup of post-pancreatitis rendez vous procedures.This group showes a significant high average operative time (217min),hospital stay (15.4 days)and postop morbility rate (7/15).No conversion in this group.A significant high average hospital stay was connected with the group of patients admitted in internistic ward without correlation with postop morbility.
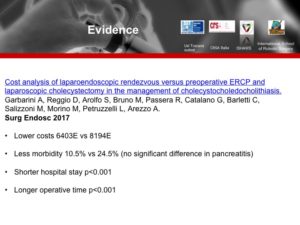
A recent prospective randomized study by Rabago LR comparing a preop ERCP group with intraop ERCP group using the rendez vous technique concludes supporting that the use of new treatment options to the management of choledocholithiasis depends more on the technical skills and experience of the endoscopic or surgical teams than on clearly established and accepted consensus.Both treatment approaches were equally effective but the rendez vous group had less morbidity,a shorter hospital stay and reduced cost.The lower morbidity in the intraop group resulted from the lower rate of papillotomy and lower rates of post-ERCP pancreatitis and cholecystitis.
References
Barr LL,’ Frame A, Couanjon A (1999) Proposed criteria for preoperative endoscopic retrograde cholangiography in candidates for laparoscopic cholecystectomy. Surg Endosc 13: 778-781
Berthou JC, Drouard F, Charbonneau P, Moussaier K (1998) Evaluation of laparoscopic management of common bile duct stones in 220 patients. Surg Endosc 12: 16-22
Carroll BJ, Fallas MJ, Phillips EH (1994) Laparoscopic transcysti choledochoscopy. Surg 8: 310-314
Carroll BJ, Phillips EH, Dayakhovsky L (1992) Laparoscopic choledoscopy: an effective approach to the common bile duct. J Laparoendosc Surg 2: 15-21
Cisek PI, Greaney GC (1994) The role of endoscopic retrograde cholangiopancreatography with laparoscopic cholecystectomy in the management of choledocholithiasis. Am Surg 60: 772-776
Coppol R, Riccioni ME, Ciletti S, Cosentino L, Ripetti V, Magistrelli P, Picciocchi A (2001) Selective use of endoscopic retrograde cholangiopancreatography to facilitate laparoscopic cholecystectomy without cholangiography. Surg Endosc 15: 12131216
Deslandres E, Gagner M (1993) Intraoperative endoscopic sphincterotomy for common bile duct stones during laparoscopic cholecystectomy.Gastrointest Endosc 39: 54-58.
Fiore NF, Ledniczky G, Wiebke EA, Broaclie TA, Pruitt AL, Goulet RJ, Grosfeld JL, Canal DF (1997) An analysis of perioperative cholangiography in one thousand laparoscopic cholecystectomies. Surgery 122: 817-821
Franciosi C, Capriotti R, De Fina S, Romano F, Colombo G, Uggeri S, Sartori P, Visintini G, Uggeri F (2000) Sequential endolaparoscopic treatment in patients with common bile duct calculi. Minerva Chir 55: 665-671
Graham SM, Flowers JL, Scott TR, Hunter J (1993) Laparoscopic cholecystectomy and common bile duct stones. The utility of planned perioperative endoscopic retrograde cholangiography and sphincterotomy: experience with 63 patients. Ann Surg 218: 61-67
Hunter JG (1992) Laparoscopic transcystic common bile duct exploration. Am J Surg 163: 53-65
Jung LU, Potter SD, Joscia MF, Gluck ES, Antonelle MA, Antonelle RW, Steichen FM, Sottile EB (1996) Laparoscopic cholecystectomy and intraoperative ERCP. Surg Rounds 19: 406-412
Kent AL, Cox MR, Wilson TG, Padbury RTA, Toouli J (1994) Endoscopic retrograde cholangiopancreatography following laparoscopic cholecystectomy. Aust N Z J Surg 64: 407-412
Lenriot JP, Le Neel JC, Hay JM, Jaeck D, Millat B, Fagniez PL (1993) Retrograde cholangiopancreatography and endoscopic sphincterotomy far biliary lithiasis. Prospective evaluation in surgical circle. Gastroenterol Clin Biol 17: 244-250
Lilly MC, Arregui ME (2001) A balanced approach to choledocholithiasis.Surg Endosc 15: 467-472
Meyer C, Vo Huu Lee J, Rohr S, Thiry LC, Duclos B, Reimund JM, Baumann R (1999) Management of common bile duct stones in a single operation combining laparoscopic cholecystectomy and perioperative endoscopic sphincterotomy. Surg Endosc 13: 874877
Paganini AM, Lezoche E (1998) Follow-up of 161 unselected consecutive patients treated laparoscopically far common bile duct stones. Surg Endosc 12: 23-29
Park AE, Mastrangelo MJ Jr (2000) Endoscopic retrograde cholangiopancreatography in the management of choledocholithiasis. Surg Endosc 14: 219-226
Paul A, Millat B, Holthausen U, Sauerland S, Neugebauer E (1998) Diagnosis and treatment of common bile duct stones (CBDS). Results of a consensus development conference. Surg Endosc 12: 856-864
Philips EH, Liberman M, Carroll Bl, Fallas MJ, Rosenthal RJ, Hia JR (1995) Bile duct stones in the laparoscopic era. Is preoperative sphincterotomy necessary’? Arch Surg 130: 880-885
Prat F, Meduri B, Ducot B, Chiche R, Salimbeni-Bartolini R, Pelletier G (1999) Prediction of common bile duct stones by noninvasive tests. Ann Surg 229: 362-368
Salm R, Waininger J, Matern U, Farthmann EH (1994) Laparoscopic techniques in therapy of choledocholithiasis. Chirurg 65: 418-423
Stain SC, Cohen H, Tsuishoysha M, Donovan AJ (1991) Choledocholithiasis: endoscopic sphincterotomy or common bile duct exploration? Ann Surg 213: 627-634
Tricarico A, Cione G, Sazio, et al. (2002) Endolaparoscopic rendezvous treatment: a satisfying therapeutic choice for cholecystocholedocolithiasis. Surg Endosc 16: 711-713 .
Trondsen E, Edwin B, Reitersen O, Faerden AE, Fagertun H, Rosseland AR (1998) Prediction of common bile duct stones prior to cholecystectomy: a prospective validation of a discriminant analysis function. Arch Surg 133: 162-166
Vracko J, Wiechel KL (1998) How often might a trans-cystic-duct stone extraction be feasible? Surg Endosc 12: 12-15
Williams GL, Vellacott KD (2002) Sclective operative cholangiography and perioperative endoscopic retrograde cholangiopancreatography (ERCP) during laparoscopic cholecystectomy. Surg Endosc 16: 465-467
Wilson TG, Hall JC, Watts JM (1986) Is operative cholangiography always necessary? Br l Surg 73: 637-640
Andriulli A, Leandro G, Niro G, Mangia A, Fesla V, Gambassi G, et al. (2000) Pharmacologic treatment can prevent pancreatic injury after ERCP: a meta-analysis. Gastrointest Endosc 5i: 1-7
Barwood NT, Valinsky LJ, Hobbs MS, Fletcher OR, Knuiman MW, Ridout SC (2002) Changing methods of imaging the common bile duct in the laparoscopic cholecystectomy era in Western Australia: implications for surgical practice. Ann Surg 235: 41-50
Berci G, Morgenslern L (1994) Laparoscopic management of common bile duct stones: a multi-institutional SAGES study. Society of American Gastrointestinal Endoscopic Surgeons. Surg Endosc 8: 1168-1174
Berthou JC, Orouard F, Charbonneau P, Moussalier K (1998) Evaluation of laparoscopic management of common bile duct stones in 220 patients. Surg Endosc 12: 16-22
Binmoeller KF, Schafer TW (2001) Endoscopic management of bile duct stones. J Clin Gastroenterol 32: 106-118
Carroll Bl, Phillips EH, Chandra M, Fallas M (1993) Laparoscopic transcystic duct balloon dilatation of the sphincter of Oddi. Surg Endosc 7: 514-517
Cavina E, Franceschi M, Sidoti F, Goletti O, Buccianti P, Chiarugi M (1998) Laparo-endoscopic “rendez vous”: a new technique in the choledocholithiasis treatment. Hepatogastroenterology 45: 1430-1435
Costamagna G, Tringali A, Shah SK, Mutignani M, Zuccala G, Perri V (2002) Long-tenn follow-up of patients after endoscopic sphincterotomy for choledocholithiasis, and risk factors for recurrence. Endoscopy 34: 273-279
Curet MJ, Pitcher DE, Martin DT, Zucker KA (1995) Laparoscopic antegrade sphincterotomy: a new technique for the management of complex choledocholithiasis. Ann Surg 221: 149-155
Cuschieri A (2000) Ductal stones: pathology, clinical manifestations, laparoscopic extraction techniques, and complications. Semin Laparosc Surg 7: 246-261
Cuschieri A, Lezoche E, Morino M, Croce E, Lacy A, Toouli J et al. (1999) E.A.E.S. multicenter prospective randomized trial comparing two-stage vs single-stage management of patients with gallstone disease and ductal calculi. Surg Endosc 13: 952-957
Decker G, Borie F, Millat B, Berthou JC, Deleuze A, Drouard F, et al. (2003) One hundred laparoscopic choledochotomies with primary closure of the common bile duct. Surg Endosc 17: 12-18
DePaula AL, Hashiba K, Bafutto M, Zago R, Machado MM (1993) Laparoscopic antegrade sphincterotomy. Surg Laparosc Endosc3: 157-160
Dickinson RJ, Davies S (1998) Post-ERCP pancreatitis and hyperamylasaemia: the role of operative and patient factors. Eur J Gastroenterol Hepatol 10: 423-428
Fitzgibbons Jr RJ, Gardner GC (2001) Laparoscopic surgery and the common bile duct. World J Surg 25: 1317-1324
Fletcher DR (1994) Changes in the practice of biliary surgery and ERCP during the introduction of laparoscopic cholecystectomy to Australia: their possible significance. Aust N Z 1 Surg 64: 75-80
F]etcher DR, Hobbs MS, Tan P, Valinsky LJ, Hockey RL, Pikora TJ, et al. (1999) Complications of cholecystectomy: risks of the laparoscopic approach and protective effects of operative cholangiography: a population-based study. Ann Surg 229: 449-457
Freeman ML, DiSario JA, Nelson DB, Fennerty MB, Lee JG, Bjorkman DJ, et al. (2001) Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc 54: 425-434
Gigot JF, Navez B, Etienne J, Cambier E, Jadoul P, Guiot P, et al.(1997) A stratified in tra operative surgical strategy is mandatory during laparoscopic common bile duct exploration for common bile duct stones: lessons and limits from an initial experience of 92 patients. Surg Endosc Il: 722-728
Himal HS (2000) Common bile duct stones: the role of preoperative, intraoperative, and postoperative ERCP. Semin Laparosc Surg 7: 237-245
Iodice G, Giardiello C. Francica G, Sarrantonio G, Angelone G, Cristiano S, et al. (2001) Single-step treatment of gallbladder and bile duct stones: a combined edoscopic-laparoscopic technique. Gastrointest Endosc 53: 336-338
Poon RT, Yeung C, Lo CM, Yuen WK, Liu CL, Fan ST (1999) Prophylactic effect of somatostatin on post-ERCP pancreatitis: a randomized controlled trial. Gastrointest Endosc 49: 593-598
Schreurs WH, Juttmann JR, Stuifbergen WN, Oostvogel Hl, van Vroonhoven TJ (2002) Management of common bile duct stones: selective endoscopic retrograde cholangiography and endoscopic sphincterotomy: short- and long-term results. Surg Endosc 16: 1068-1072
Sherman S, Hawes RH, Ralhgaber SW, Uzer MF, Smith MT, Khusro QE, et al. (1994) Post-ERCP pancreatitis: randomized, prospective study comparing a low- and high-osmolality contrast agent. Gastrointest Endosc 40: 422-427
Stein DE, Sclafani SJ, Kral JG (1998) Management ofT tubes for common bile duct stones: a new technique. Dig Surg 15: 279-282
Tranter SE, Thompson MH (2002) Comparison of cndoscopic sphincterolomy and laparoscopic exploralion of the common bile duct. Br 1 Surg 89: 1495-1504
Urbach DR, Khajanchee YS, lobe BA, Standage BA, Hansen PD, Swanstrom LL (2001) Cost-effective management of Common bile duct stones: a decision analysis of the use of endoscopic retrograde cholangiopancreatography (ERCP), intraoperative cholangiography, and laparoscopic bile duct exploration. Surg Endosc 15: 4-13
Vecchio R, MacFadyen BV (2002) Laparoscopic common bile duct exploration. Langenbecks Arch Surg 387: 45-54
Enochsson L,Lindberg B,Swahn F,Arnelo U (2004) Intraoperative endoscopic retrograde cholangiopancreatography (ERCP) to remove common bile duct stones during routine laparoscopic cholecystectomy does not prolong hospitalization.Surg Endosc 18:367-371
Saccomani G,Durante V,Magnolia MR,Ghezzo L,Lombezzi R,Esercizio L,Stella M,Arezzo A (2005) Combined endoscopic treatment for cholelithiasis associated with choledocholithiasis.Surg Endosc 19:910-914
Basso N, Pizzuto G,Surgo D,Materia A,Silecchia G,Fantini A,Fiocca F,Trentino P (1999) Laparoscopic cholecystectomy and intraoperative endoscopic sphincterotomy in the treatment of cholecysto-choledocholithiasis Gastrointest Endosc 50:532-535
Lacitignola S,Minardi M,Palmieri R,Nigri A,Caliandro L,Rosellini A (2005) A “one-stage” laparoscopic procedure for treating choledocholithiasis JSLS 9:419-421
Rabago LR,Vicente C,Soler F,Delgado M,Moral I,Guerra I,Castro JL,Quintanilla E,Romeo J,Llorente R,Vazquez J,Martinez JL (2006) Two-stage treatment with preoperative endoscopic retrograde cholangiopancreatography (ERCP) compared with single-stage treatment with intraoperative ERCP for patients with symptomatic cholelithiasis with possible choledocholithiasis Endoscopy 38:779-786
Clayton ESJ,Connor S,Alexakis N,Leandros E (2006) Meta-analysis of endoscopy and surgery versus surgery alone for common bile duct stones with the gallbladder in situ.Br J Surg 93:1185-1191
Boerma D,Schwartz M (2006) Management of common bile-duct stones and associated gallbladder stones:surgical aspects.Clin Gastroenter 20:1103-1116
National Institutes of Health (2002) Endoscopic Retrograde Cholangiopancreatography (ERCP) for diagnosis and therapy NHI 19:1

Quest’opera è distribuita con Licenza Creative Commons Attribuzione – Non commerciale – Non opere derivate 3.0 Italia.
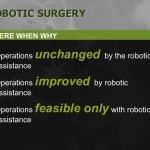
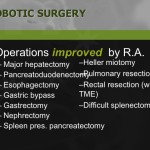
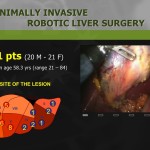
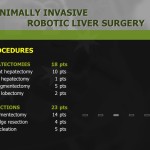
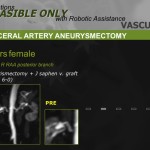
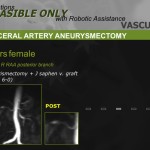
update in chirurgia robotica

Quest’opera è distribuita con Licenza Creative Commons Attribuzione – Non commerciale – Non opere derivate 3.0 Italia.